free men
فريق العمـــــل *****
التوقيع : 
عدد الرسائل : 1500
الموقع : center d enfer
تاريخ التسجيل : 26/10/2009
وســــــــــام النشــــــــــــــاط : 6
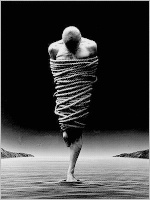
 | |  The Impact of Disability on Well-Being: What is at Stake? The Impact of Disability on Well-Being: What is at Stake? | |
This subsection will examine how assumptions about the relationship between disability and well-being that have been challenged in academic debate continue to play a significant role in reproductive and health-care decision making. We discuss four contexts in which these assumptions have been relied upon in policies and personal decisions about creating or sustaining lives: reproductive testing for disability, neonatal care, “end-of-life“ decision making, and the use of ”quality-adjustment” measures to assess the cost-effectiveness of health-care and other interventions.In all of these cases, objections have been raised besides those concerning the assumption that lives with serious disabilities must be substantially worse than lives without them. For example, in the case of life-termination, the debate also concerns the decisional capacity of newly disabled individuals; in the case of quality-adjustment, the debate also concerns the assumption that the quality of a life should affect its priority in allocating scarce resources. We will, however, focus on the objections that concern well-being.1.5.1 Reproductive testingSome prospective parents see life with some disabilities as worse than no life at all. This claim is often made with respect to such conditions as Tay-Sachs, Lesch-Nyan, and trisomies 13 and 18. Even for those conditions, however, that view is not universally held (Wilkinson 2011). The notion of a life so bad that it is a harm to the individual living it came to popular and philosophical attention in the 1980s, when a number of lawsuits in the U.S claimed that physicians or parents had wronged the child by failing to diagnose its condition in utero and/or prevent its birth. These lawsuits appeared to require a comparison of existence and non-existence, which most courts and some philosophers rejected. A majority of philosophers, however, starting with Joel Feinberg (1986), have concluded that the notion can be useful in theory if not necessarily in practice.In cases involving less severe disabilities, some prospective parents think that they are protecting the welfare of “their child” by preventing the existence of a child who would have a disability. This attitude involves seeing the future child not as a particular individual who can only exist with a disability, but as a role that prospective parents do not want to fill with a disabled child. Philosophers have debated the appropriateness of regarding future children in this way (Malek 2008; Hare 2007; Velleman 2008; Wasserman 2008; Heyd 2009). Even if this view were appropriate, its moral force would depend on the extent to which the diagnosed condition could reasonably be expected to reduce the child’s welfare, as well as the existence and strength of a moral reason not to bring into existence persons with such welfare deficits.In the context of prenatal testing, as with assessments of adult functioning, the extent to which a disabling condition reduces well-being depends on the conception of well-being that is adopted. With prenatal testing, however, there is an additional complication: there is massive uncertainty about how the detected variants will be expressed in the developing child. That depends on their their interplay with other genes and interaction with a variety of environments. The formidable challenges of predicting phenotype may be more readily acknowledged by health professionals than the even more daunting challenges in the non-medical assessment of how life with a given phenotype could go for the person living it.1.5.2 Withdrawal of Life Support from Disabled NewbornsThe debate over the withdrawal of life support for very premature and severely disabled newborns surfaced in the 1980s with the 1982 Bloomington, Indiana Baby Doe case and the adoption of federal guidelines for support of newborns and termination of life-sustaining treatment. The debate continues as medical technology permits an increasing number of severely disabled newborns to survive. Some of the debate appears fairly abstract, concerning whether there should be a “grey area” around “a life (just barely) worth living”, in which parents and physicians would be permitted to decide for themselves whether to continue or withdraw life-support (Wilkinson 2011). Disability scholars, however, have the more practical concern that decisions about life-support, whether made by parents or caretakers, too often rely on inaccurate or misleading medical indicators of expected well-being, resulting in significant discrimination against newborns with disabilities (Silvers and Francis 2011). Although the accuracy of medical prediction may improve after birth, it remains difficult to assess the potential of a neonate to develop higher cognitive functions. And although the prediction of the course of physical impairments has improved, that improvement offers only a partial safeguard against the tendency of many parents and health professionals to exaggerate the hardships of life with an impairment—a tendency driven as much by stigma as by medical error and uncertainty.1.5.3 “End-of-Life” Decision MakingAssumptions about disability and well-being play an important if somewhat less salient role in this context. They figure most prominently when the individual is no longer capable of deciding for herself whether to receive, continue or refuse life-sustaining treatment. For adults once capable of making such decisions, two standards apply to surrogate decision making: substituted judgment and best interest. The first involves judging what the individual would have wanted or chosen if she could want or choose for her current situation; the second involves judging the person’s interests by a standard other than her own. In cases where the adult never had decisional capacity and there is no basis for making a judgment about what the patient would have chosen, the best interest standard applies. But those who judge the best interests of such an adult are prone to the same errors of projection as nondisabled people judging the well-being of disabled people. A nondisabled surrogate might be devastated at losing capacities the cognitively impaired individual never had, or assume that the inability to understand the source of, or reason for, physical pain must be even more traumatic for that individual than it would be for the surrogate. Such judgments are not clearly wrong, but rather speculative; the primary error is in overconfidence.Assumptions about disability and well-being also play a significant role in judging the reasonableness of requests by competent adults to end, or not receive, life sustaining treatment. Many jurisdictions recognize the right of such individuals to make this decision for themselves, but disability advocates remain concerned that their decisions are more likely to be considered reasonable, and respected, if they are made in response to severe, permanent disabilities. Thus, in the influential case of Elizabeth Bouvia, the court allowed a fully competent, severely disabled, women to refuse the medical support that could have prolonged her life indefinitely. Critics of the decision maintained that both Bouvia and the court were unduly swayed by the perceived indignity of her physical dependence, and by their difficulty in seeing how life could go very well with a severe disability (Asch 2005; Gill 1992; Longmore 1987).1.5.4 Health Related Quality-of-Life MeasuresPerhaps the setting in which the relationship of disability to well-being has received most attention is the assessment of “quality of life” (see, generally, Wasserman, et al. 2005a). For judging the cost-effectiveness of medical interventions, it is useful to have measures of well-being that facilitate quantitative comparison. Quality-of-life measures in medicine and health care offer benchmarks for assessing the well-being of groups of people, focusing on the aspects of well-being most amenable to reliable assessment. There is no guarantee that individuals who are doing well by such measures are actually living good lives according to more robust philosophical criteria of well-being. Any uniform metric for quality of life will provide an oversimplified assessment of an individual’s well-being, and to some extent this is unavoidable from a policy perspective. But the worry when these judgments are applied to people with disabilities is not oversimplification so much as systematic bias.Assumptions about the adverse effect of disability on well-being pervade the measurement of “health-related quality of life” (HRQL). In particular, two features of many standard approaches to measuring HRQL treat disability as inimical to well-being: 1) assuming that an individual’s adaptation to a disability is a source of distortion or a measurement artifact in assessing how well he or she is doing; 2) expanding the definition of health outcomes to include not only the physiological and sensory-motor effects of disease and injury, but their “sequelae”—their effect on daily living and social participation. The first feature ignores the extent to which adaptation involves changes that would count as improvements in well-being on most objective as well as subjective accounts (Menzel et al. 2002; Barnes 2009a). The second fails to distinguish the contribution of medical and social/environmental factors to the restriction or loss of objectively valuable activities (Wasserman, et al. 2005a). These features not only exaggerate the adverse impact of disabilities, but in some contexts, threaten adverse consequences for people with disabilities.The inclusion of functional and activity limitations as health outcomes is in tension with the social model of disability, which treats many of those limitations as due to an exclusionary environment. It also conflicts with the view, discussed below, that an individual can be disabled but healthy. The assumption that adaptation to disability cannot be an accurate measure of well-being has motivated a reliance on health professionals to assess the quality of life with specific disabilities, rather than on people with those disabilities (Murray 1996). The refusal to treat people with disabilities as reliable witnesses to, or authorities on, their well-being is particularly striking, given that nondisabled people also adapt to the vicissitudes of their lives (Brickman and Campbell 1971). As Wasserman, et al. note: - اقتباس :
- The lives of people with disabilities are assumed to be of low quality, whatever environmental factors mediate the impact of their impairments, and their own testimony to the contrary is seen as inherently unreliable. Their adaptations to their impairments appear not as instances of the universal processes of adjustment to changed circumstances, but as disability-specific strategies for recovering the ground that has been lost, or for covering up its loss through benign self-deception (2005a: 11).
This view of disability is not merely inaccurate. Its use to assess the effectiveness of health care interventions has disturbing implications for the lives of people with disabilities. Effectiveness measures typically treat a disability as equivalent for assessment purposes to a shorter life-span. Health outcomes are measured by life-years saved or gained; life-years are “adjusted” by their quality, and their rated quality is substantially reduced if the intervention fails to correct, risks causing, or causes a disability. As a result, people who have, or will be left with, disabilities also have their future life-years adjusted downward in light of the presumed lower quality of those life-years. As a result, the priority of persons with disabilities for life-saving interventions is substantially reduced. Because it employed such discounting, the 1990 Oregon Health Care Plan to set priorities for Medicaid-funded procedures was found to discriminate against people with disabilities (Bodenheimer 1997). Several years later, the most comprehensive international effort to develop summary measures of population health proposed a more explicit and very sharp discounting of lives with disabilities in assessing the “Global Burden of Disease” and in setting priorities for its reduction (Murray 1996). Although some objectionable features of the discounting methodology have been modified (Saloman and Murray 2002), the Global Burden of Disease frameworks continue to adopt procedures that result in strikingly low quality-of-life estimates for many disabilities.Many mainstream philosophers and bioethicists question the use of summary health measures in priority setting (Harris 1987; Brock 1995). They argue that their proposed use is based either on a questionable utilitarian assessment of lives as more valuable if they “contain” more utility, or on the controversial distributive principle that society should give scarce goods to those who will benefit most from them. But many still defend the general assumptions about disability and quality of life that informed those measures (Brock 2005). Other philosophers and disability scholars have challenged these assumptions (Bickenbach 2005). Some have gone even further, questioning whether quality-of-life assessments place an exaggerated premium on the prevention or correction of impairments that do not, in hospitable environments, preclude rich and rewarding lives (Barnes 2009a; Asch and Wasserman 2010). | |
|


