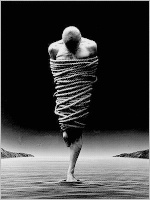
free men
فريق العمـــــل *****
التوقيع : 
عدد الرسائل : 1500
الموقع : center d enfer
تاريخ التسجيل : 26/10/2009
وســــــــــام النشــــــــــــــاط : 6
 | |  Disability and Health Disability and Health | |
People appear to regard health as one of the most important goods, more important than wealth, status, or professional success. Health is seen as special in part for instrumental reasons, because it is thought to be a prerequisite for many or most other goods. So the relationship of health to disability is an issue of central concern for those who seek to replace or supplement a medical model of disability (Bickenbach 1993; Shakespeare 2006).The social model of disability, which informs the Americans with Disabilities Act and kindred legislation, may appear to move disability away from health policy and toward civil rights. Yet movement in one direction does not preclude movement in the other. People with disabilities have significant health care needs, and their needs may depend to some extent upon their disabilities. For philosophers as well as policy makers, the challenge posed by the social model is to acknowledge the importance of health and health care for people with disabilities without assuming that all people with disabilities are unhealthy just because they are disabled, and without overemphasizing the correction or mitigation of impairments. This requires a careful examination of the relationship between health and disability. Do all disabilities result from, or in, a loss of health? Can a person with a disability be in good or even “perfect” health? To answer such questions, we need a serviceable theory, concept, or definition of health.There are a variety of competing philosophical accounts of health (see SEP entry on concepts of health and disease). They can be distinguished in several ways: 1) some regard health as the mere absence of disease (e.g., Hofman 2005); others regard health as a form of well-being or flourishing, and treat the absence of disease as at most a necessary condition of health (e.g., Carel 2007 and WHO 1948); 2) some regard the concept of health as value-laden, or normative, in the sense that the good of health enters into its very concept (e.g., Engelhardt 1986; DeVito 2000); others regard health as value-neutral, or non-normative, defined by bio-statistical or other biological criteria (e.g., Boorse 1987 and Wachbroit 1998); 3) some see the value of health as instrumental, in the capacity of the agent or organism to achieve certain goals (e.g., Nordenfeldt 1995); others see its value as intrinsic as well, as good in itself (e.g., Becker 2005).These distinctions are not independent of each other. Non-normative accounts of health tend to treat health as the absence of disease, dysfunction, or deformity. These accounts also tend to be instrumental: they define health as normal or species-typical biological functioning, which is itself defined in such goal-oriented terms as survival and reproduction. On the other hand, instrumental accounts that define health in terms of the pursuit of an individually, culturally, or other variable range of goals will tend to weaken the connection of health to bodily, cognitive, or affective functioning.If health is defined simply as the absence of disease, then a person can be disabled but healthy if and only if he can be disabled but not diseased. If, however, health is a state of psychophysical flourishing or vitality, then an individual can be healthy, although perhaps not perfectly healthy, even if disabled or diseased, and unhealthy even if free of disability or disease.Many philosophers and bioethicists take it that “health”, “disease”, and “disability” are value-laden, that it is part of their meaning that the conditions to which they refer are (inherently) desirable or undesirable (e.g., Engelhardt 1986 and DeVito 2000). Two notable exceptions are Christopher Boorse and Robert Wachbroit, who offer biomedical definitions that are value-neutral, or as Boorse claims, as value-neutral as biology itself (Boorse 1987: 359–93; Wachbroit 1998: 533–38). They define health in terms of normal or species-typical physical and mental functioning, so that disabilities are by definition unhealthy. But such value-neutral accounts do not assume that disabilities are therefore bad or undesirable, merely atypical.[2]Since they deny that the goodness of health is part of its definition, value-neutral accounts stress the enormous, but contingent, instrumental value of health. The leading attempt to explain the importance of health in these terms is Daniels’ account of health-care as maintaining or restoring fair equality of opportunity (Daniels 1985). Daniels’ account gives a priority to the maintenance of typical functioning and the correction of disabilities that many critics find excessive (Wasserman 1998: 152–58). Still, the core intuition, concerning the enormous practical value of species-typical functioning, can be accepted without accepting medical normalization as the preferred or default response to atypicality; indeed, without accepting the claim that species have functions with species- typical levels defined in biological terms (see Amundson 2000). Further, the claim that species-typical functioning is instrumentally valuable leaves open the question ofwhy departures from species-typical functioning are instrumentally disvaluable: is it because they render one vulnerable to discrimination, subject one to an unaccommodating environment, cause medical problems, or all of the above?Yet most people have a strong conviction that practical advantages do not exhaust the value of health, nor practical disadvantages its disvalue. To accommodate this conviction, those accepting a narrow definition of health as the absence of disease may want to acknowledge that disease, or its usual symptoms or consequences, has inherent disvalue, while distinguishing disability from the other symptoms or consequences of disease, particularly pain and death. Those adopting a broader definition of health as an aspect of well-being or flourishing may also want to claim that being unhealthy has inherent disvalue, while distinguishing disability from a lack of health. 2.1 The First Approach: Distinguishing Disability from DiseaseThe distinction between disease and disability has received surprisingly little attention in the philosophical literature. Most statutory and other official definitions either treat serious diseases as disabilities or make “impairment”, “loss of function”, or “structural/functional abnormality” an element of disability, leaving the relationship of disease to disability unclear (e.g., Americans with Disabilities Act, 1990 or Disability Discrimination Act, 1995). One of the few detailed analyses of the relationship between disease and disability was offered by Ron Amundson, who proposed that disability should be understood as one of the three general consequences of disease, along with pain and death (Amundson 1992: 105–119). Amundson adopted Boorse’s value-neutral account of health, but argued that Boorse defined “disease” too broadly, as a “deviation from the functional organization of typical members of a species”—a definition which would encompass most disabilities. Amundson contended that it was both clearer and closer to common usage to treat disease as an atypical process that tended to result in disability, pain, or death.[3]Amundson defined disability as the loss or deviation from a particular kind of species-typical function: action at the personal level, e.g., the inability to move one’s arm, as opposed to the inability to metabolize sugar. Disabilities that are not products of a process that leads to pain, death, or further impairment are not symptomatic of disease in Amundson’s sense. They are consistent with health narrowly defined. Yet some philosophers (Hausman 2001: 254) find the notion that individuals can be in excellent health if they are blind, deaf, or paraplegic sufficiently implausible to count against analyses of health with that implication.The disagreement between Amundson and Boorse on the distinction between disease and disability is not just a matter of semantics. The critical point in Amundson’s analysis is a practical one. Medical interventions are the presumptive response to disease; they seek to slow, arrest, or reverse processes that cause pain and may lead to physiological dysfunction, (further) disability (in Amundson’s terms), or death. But on Amundson’s view, which makes disability consistent with health, the presumptive response to disability need not be medical as opposed to environmental or social. Furthermore, the loss of opportunity associated with disabilities can often be prevented or mitigated more effectively and (in the long run) more economically by modifying the physical and social environment than by medical intervention. This is true even though environmental measures are likely to fare poorly against medical interventions in the competition for scarce resources, because of the prestige and perceived importance of medical treatment. The failure to distinguish disease and disability, and the tendency to favor a medical response for both, reflects the sway of the medical model, and offers a clear illustration of how it differs from the social model (see SEP entry on disability: definitions, models, experience).Recently, Peter Hucklenbroich has proposed a harm-oriented account of health as the absence of a “disease” process. Such a process is pathological in the sense that:[list="margin-top: 0.5em; color: rgb(26, 26, 26); font-family: serif; font-size: 16.5px; line-height: 21px; background-color: rgb(255, 255, 255);"] [*]it is immediately lethal or definitely life-shortening, [or] [*]it is a condition of pain, suffering, or other specific complaints, [or] [*]it is a condition of infertility (incapability of biological reproduction), [or] [*]it is a condition of inability or impairment for living together in human symbiotic communities, [or] [*]it is a non-universal disposition of the organism to develop a condition that is pathological according to one or more of these criteria. (12) [4][/list] Hucklenbroich’s account defines health in terms of a list of reasonably health-specific harms and it restricts health to the absence of biological conditions that either (a) directly involve harm or (b) dispose one to suffer harm.An account along these lines may have the potential to distinguish disease from disability so as to make the former immediately relevant to well-being in a way the latter is not. Unlike purely non-normative accounts, it only finds a health-decrement where something bad comes from the state of the body. Unlike capaciously normative accounts, it defines these “bads” in terms of a general and health-specific harm; not just any body-based limitation on the pursuit of our (potentially idiosyncratic) goals makes us unhealthy. And finally, defining health in terms of bodilydispositions could help to explain why extrinsic factors, like those cited by social models of disability, are irrelevant to health. It could distinguish between harms that come from social responses to the body from harms that come from the body itself; thereby distinguishing between harms that generate claims on health care and harms that generate claims against discrimination or the denial of fair equality of opportunity.Despite the importance of distinguishing disease from disability, there are at least three reasons why it is difficult to do so. First, as noted above, many or most diseases are defined as disabilities by disability discrimination laws or their judicial and administrative interpretations; they are subject to the same legal protections and requirements of reasonable accommodation as “Amundsonian” disabilities. This legal treatment may, however, be justifiable, because some diseases, such as AIDS, are stigmatized as severely as many or most disabilities. Second, many disabilities, such as the inability to walk, may be associated with diseases, such as MS, which have a progressive character, causing pain and further impairment, and sometimes increasing the risk of death (Wendell 2001).[5] Third, a society such as our own, where atypical functionings are often not well accommodated, accords a higher priority to the prevention or treatment of some non-fatal diseases than would a society that better accommodated them. | |
|


